Dysphonia is a voice disorder manifested by weakness, hoarseness, and hoarseness. With complete loss of voice, aphonia is diagnosed. In this case, a rattling sound appears in speech, but the ability to speak in a whisper remains. Dysphonia can occur at any age for various reasons; it has a pronounced clinical picture, thanks to which the diagnosis is determined quite accurately. At the same time, it responds well to complex treatment. There are two main forms of dysphonia: functional and organic.
1.General information
The term “dysphonia” in translation and essentially means a disorder of phonation, i.e. purely acoustic, vocal components of speech.
Dysphonic syndrome, developing outside of acute inflammation of the laryngopharynx, has long been considered a disorder of the neurotic, hysterical register, but today it has been established that the etiological structure of dysphonia (and aphonia as a complete absence of voice) is much broader.
The prevalence of dysphonia also varies widely in different statistical samples. According to modern estimates, dysphonia of varying severity is diagnosed with a frequency of 1-40% in children and 2-50% in adults. Representatives of speech and vocal professions (singers, teachers, conversational artists, etc.) suffer from dysphonia much more often than any other category of the population, and this constitutes a serious socially significant problem in any country.
A must read! Help with treatment and hospitalization!
Forecasts
Dysphonia goes away forever if help comes on time and the rehabilitation plan is drawn up correctly. Difficulties arise if the patient is again faced with a traumatic factor, if psychological problems are added to this (lack of faith in one’s own strengths and the possibilities of therapy), or if the treatment process has been delayed.
The NeuroSpectrum Center for Children's Speech Neurology and Rehabilitation offers a full examination for the presence of dysphonia, consultations with specialized specialists, as well as comprehensive treatment. Together we will restore the voice, return its timbre and tonality.
2. Reasons
There are two fundamentally different forms of dysphonia: organic and functional.
Organic dysphonia is usually caused by inflammatory processes in the larynx and upper respiratory tract, abnormalities of intrauterine development, angiomas, traumatic and iatrogenic factors.
Functional dysphonia can be caused by:
- severe stressors (reactive dysphonia) and psychoneurological pathology (neurogenic dysphonia/aphonia, mutism in hysteria, schizophrenia, etc.);
- vertebrological, cardiovascular, pulmonological, endocrine diseases;
- occupational hazards (vocal apparatus overload);
- deficiency of vitamins and microelements;
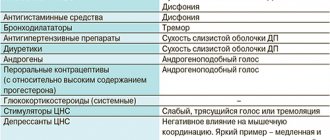
- taking certain groups of medications (in particular, hormone-containing ones).
Hypotonic (non-closing ligaments) dysphonia is caused by functional insufficiency (decreased elasticity, tone, activity) of the muscles and ligaments of the larynx responsible for phonation processes. The cause is often, in particular, age-related degenerative-dystrophic changes in tissue.
Hypertonic dysphonia is associated with pathological, excessive, usually painful closure of the vocal cords (for example, in spastic conditions of the larynx, some neurological diseases, etc.).
Mixed hypo-hypertonic dysphonia is also found. Mutational dysphonia (the so-called “voice breakdown”) of the puberty period is considered as a special form. Contrary to popular belief, normal mutational dysphonia is observed in adolescents not only males, but also females.
It should be noted that in some cases, dysphonia turns out to be a polyetiological disorder, i.e. caused by several of the listed reasons simultaneously.
Visit our Otolaryngology (ENT) page
Survey
Patients who have problems with their voice should visit an otolaryngologist-phoniatrist. Also, if indicated, consultation with a neurologist, endocrinologist, or psychologist is necessary. To clarify the diagnosis you will need:
- endoscopy of the larynx;
- acoustic voice analysis;
- electroglottography;
- electromyography;
- blood analysis;
- bacterial culture from the nasopharynx;
- biopsy;
- tracheoscopy.
It is also necessary to be examined by a speech therapist. For functional dysphonia, treatment is prescribed by a phonopedist. Diagnostics will help to clearly determine the subtype of the disease, which is important for determining treatment tactics. Our Center’s specialists are ready to accept patients with this disease and provide the necessary assistance.
3. Symptoms and diagnosis
By definition, dysphonia is manifested by distinct changes in timbre, volume, acoustic purity, and individually normal voice tonality.
Sometimes, depending on the etiology (inflammation, laryngospasm), there is more or less painful phonation and swallowing, as well as a stridorous (noisy whistling) component in breathing. Patients with hypotonic dysphonia often notice fatigue of the vocal apparatus.
Diagnosis is carried out through careful collection and analysis of complaints, general anamnestic information, and data on the dynamics of the condition.
Physical methods include laryngoscopy, x-rays, ultrasound, tomographic studies, laboratory tests, phoniatric tests.
As necessary, specialized specialists (endocrinologist, surgeon, psychoneurologist, etc.) are involved in the examination, as a result of which a patient who turns to an otolaryngologist often must be redirected for treatment to another doctor.
About our clinic Chistye Prudy metro station Medintercom page!
Dysphonia Treatment Methods
Treatment for dysphonia involves medication and physical therapy. Patients with a functional type of disorder (including somatics) can be absolutely healthy. Then medications are simply not needed.
So, treatment of hypotonic dysphonia means that the doctor will prescribe B vitamins. For the hypertonic version of the disorder, they will prescribe some kind of sedatives and antispasmodics. Homeopathic remedies are often used to relieve symptoms.
In the functional form of dysphonia, good results are achieved by external procedures: electrophoresis, amplipulse therapy, magnetic therapy. If necessary, the laryngeal mucosa is directly affected. For this purpose fluctuarization is used.
Inhalations and drip administration of medications directly onto the walls of the larynx help well. Ozone therapy is useful. To relieve muscle spasms in the muscles of the neck and larynx, botulinum toxin injections are given.
To normalize the psycho-emotional sphere and nervous system, acupuncture and massage are prescribed. Perhaps you need the help of a psychologist or psychotherapist. Autogenic training, psychotherapy, and the use of relaxation techniques help with dysphonia.
To restore the voice, phonopedic correction is necessary. The patient will have to strengthen the vocal apparatus and laryngeal muscles, and learn proper breathing. He needs to do breathing and articulation exercises, speech therapy massage, and special exercises.
4.Treatment
The therapeutic strategy for dysphonia is based on diagnostic results.
Obviously, the main task is to treat the underlying disease (if there is one) or eliminate the immediate anatomical cause of phonation disorders (if this is possible in principle). A gentle regime is almost always necessary, as well as certain physiotherapeutic procedures, which usually bring significant relief and improvement in voice function. In some cases (developmental anomalies, tumors, etc.), the only truly effective way to achieve normophonia is surgical intervention, which today is sought to be performed in the least invasive method applicable in a particular case (for example, endoscopic).
Functional dysphonia
Functional dysphonia is diagnosed when the vocal cords cannot close without inflammation. This condition is most often caused by neurological, endocrine or psychological disorders. There are different types of this form of the disease:
- Hypotonic dysphonia. The tone of the vocal folds decreases and they do not close completely. The voice weakens and hoarses. Often occurs in older people due to age-related changes.
- Hypertonic dysphonia. The vocal folds have increased tone and are completely closed. Because of this, constant tension is formed in the abdominal and neck muscles. Pain and hoarseness develop in the larynx, and the patient constantly feels the urge to cough.
- Hypo-hypertonic. Characteristic features include relaxation of the vocal cords and tension of the vestibular cords. The voice roughens and becomes choked. The mouth feels dry and breathing may become uneven.
- Spasmodic dysphonia. It is formed as a result of psychological trauma as a result of prolonged overstrain of the muscles that are involved in inhalation and sound production. Speech is unintelligible, trembling, hoarseness, distortion and unclear sounds appear. This form can develop in parallel with other diseases in which there is excessive muscle tension.
- Psychogenic. Appears after long-term psychological or emotional stress, such as stress or depression, fears. The voice is hoarse, the emotional state is unstable.
- Mutational. Formed in adolescents during puberty, due to mental disorders in adults. There is a change in the voice for a long time with an uncontrollably changing tone.
What does speech therapy work for dysphonia involve?
Classes with a speech therapist will help cope with voice disorders and restore normal speech.
Corrective measures include exercises:
- aimed at developing correct breathing during a conversation;
- articulation gymnastics;
- breathing exercises;
- phonopedic tasks;
- exercises that stimulate coordination of phonation.
For children, all classes are conducted in an easy, playful way, so as not to cause additional tension and stress. A skilled speech therapist will turn the mandatory articulation gymnastics into a funny tale about the Tongue’s travels, and breathing exercises into an entertaining game.
Exercises for coordinating the pronunciation of sounds are based on the principle of repeating the same words or combinations of sounds, first silently, but with increased articulation, then in a whisper, and again loudly. Having learned to control phonation, the child will be able to maintain vocal mode and protect the cords.
Breathing exercises can also be a fun activity. The speech therapist will encourage the child to blow on cotton balls, blow soap bubbles, and even play musical instruments. Dynamic gymnastics expands the child's control over his breathing.
During classes, children learn to speak with different strength, intonation, duration and pitch of the voice, which allows them subsequently not only to get rid of dysphonia, but also to avoid its recurrence thanks to self-control. Learn more about how speech therapist-defectologist classes work.
Spasmodic dysphonia. Etiopathogenesis. Methods of therapeutic and corrective influence
Introduction
The problem of voice disorders in recent years has become increasingly socially important, since according to domestic and foreign authors, there has been an increase in the incidence of the vocal apparatus in the Russian Federation from 15–20% in the 30–60s to 25–30% in the last decade [ 2].
According to the All-Russian Scientific and Methodological Center for Phoniatrics, the prevalence of diseases of the vocal apparatus in various regions of Russia, according to data from visits to phoniatric offices, averages 45% [2]. Every year, 2% of residents who apply are diagnosed with a neurological disorder - dystonia, which is expressed in involuntary movements of the vocal folds [6]. There are two types of this disorder. The adduction type of spasmodic dysphonia is characterized by the fact that during the pronunciation of a sound the vocal folds close together, which occurs in 85–90% [6] of cases. With the abduction type of spastic dysphonia, the vocal cords, on the contrary, open.
Typically, spasmodic dysphonia occurs in adults aged 30–40 years [5]. The cause of this disease has not yet been fully studied, just as the factors influencing the occurrence of this pathology have not been clarified. But it is known for certain that this disease is not inherited.
This trend can be explained by stressful situations in everyday and social life, psychological trauma, stress overload, and overstrain of the vocal cords.
The main causes of this type of voice disorder can be divided into: biological
(concomitant diseases of the neuromuscular vocal apparatus),
professional
(intensity of vocal load),
domestic
(living conditions),
psychogenic
(conflict situations of various origins, psycho-emotional shocks). Often there is a combination of two or more factors that cause this voice disorder. It is important to note that this disease [5] (spasmodic dysphonia) has a devastating effect on communication and in some cases actually renders the patient mute.
In this regard, the study of spasmodic dysphonia, its neurological basis, and the exact location of the lesion is currently an important stage for the development of clinical and psychological ideas of modern specialists in the field of phonopedia, phoniatrics, otorhinolaryngology and neurorehabilitation.
The above data determine the relevance of this study.
Purpose
This work is to study the mechanisms of occurrence of spasmodic dysphonia.
Object
research is the voice and vocal function in general in spasmodic dysphonia.
Subject
research is the specifics of the development of a neurological disorder such as dystonia.
In accordance with the purpose, subject and object of the study, the following tasks
:
1. Analyze and summarize scientific and methodological literature data regarding the frequency of occurrence of this disorder;
2. To study the clinical picture, etiology/factors of occurrence of spasmodic dysphonia using the available data;
3. Based on theoretical data, identify the specifics of the pathogenetic mechanism of the presented disease;
4. Conduct an analysis of methods aimed at corrective action in terms of restoring vocal function in case of spasmodic dysphonia.
Incidence of spasmodic dysphonia
Spasmodic dysphonia usually affects women approximately twice as often as men, and on average this disease begins at the age of 45–50 years [6]. Neurologically, such patients are normal, but they often experience facial twitching or grimacing during conversation. In everyday situations, vocal symptoms are certainly present, but, interestingly, are absent when patients sing or laugh and when they are surprised or intoxicated. This observation suggests that spasmodic dysphonia is a manifestation of a psychoneurotic or conversion reaction. This disease has a devastating effect on communication and, in severe cases, actually renders the sufferer mute. It is now known that the cause of spasmodic dysphonia is neurological, but the exact location of the lesion is still debated by scientists. The deficit appears to be in proprioceptive control of the vocal cords.
Etiology of spasmodic dysphonia. Clinical picture
Spasmodic dysphonia is a voice disorder in which the predominant symptom is a voice of a tense, compressed quality, called overcompressed. Laryngoscopy in this case reveals excessive adduction of the real (sometimes false) vocal cords during phonation [4]. Excessive and inappropriate adduction of the vocal cords causes such tension that the patient has to force sounds out of the larynx.
Hyperkinetic (spastic) dysphonia is characterized by a state of spastic hyperkinesis of the laryngeal muscles with a predominance of tonic spasm.
During phonation, there is a convulsive convergence of the vocal cords and folds of the vestibule. The vocal folds are not changed, they are mobile, and during phonation they are in a state of sharp tension. The onset of spasmodic dysphonia is usually acute, usually caused by mental trauma, which in some cases is preceded by prolonged voice overstrain. The disease of spasmodic dysphonia is persistent and long-lasting and has a negative impact on the mental state of patients.
Having begun gradually, laryngeal dystonia (spasmodic dysphonia) slowly progresses over 2–4 years, after which, as a rule, it becomes stationary. As the disease progresses, other focal dystonic syndromes sometimes appear (blepharospasm, oromandibular dystonia, spasmodic torticollis, writer's cramp), sometimes postural or postural-kinetic tremor [5, 6].
The appearance of at least one of the listed syndromes facilitates the diagnosis of spasmodic dysphonia. The diagnosis is beyond doubt in cases where spasmodic dysphonia develops in the picture of generalized torsion dystonia.
The dynamic nature of dysphonia, characteristic of laryngeal dystonia (as well as other variants of dystonia), is of important diagnostic importance. The severity of dysphonia noticeably decreases after a night's sleep (especially in the first stage of the disease), drinking alcohol, and also during certain actions, such as singing, laughing, crying.
Sometimes the voice improves significantly in the first minutes of a telephone conversation, during sleep speaking, recitation, or whispered speech (paradoxical kinesia). At the same time, it is very typical to increase the severity of spasmodic dysphonia in a situation of emotional stress, after intense vocal stress, at the end of the working day.
In patients with laryngeal dystonia, one can often observe the phenomenon of “corrective gestures” [5] in the form of individual techniques, with the help of which the patient can temporarily reduce the manifestations of spasmodic dysphonia and improve the quality of speech (for example, pressing on the area of the thyroid cartilage or lifting it upward with fingers, pressing to the area of the angle of the lower jaw, etc.).
However, in general, the phenomenon of corrective gestures in spastic dysphonia is less pronounced than in spastic torticollis, and its identification requires a targeted interview and examination of the patient.
Patients with spasmodic dysphonia often experience tremor, which can have different localization and involve the vocal folds, head, lower jaw, and limbs. When localized in the extremities (usually in the hands), the trembling is postural in nature. However, tremors of the vocal folds are most often observed. In cases of isolated tremors of the vocal folds (in the absence of tremor of another localization), laryngeal dystonia must be differentiated from isolated tremor of the vocal folds (without dysphonia), which is a variant of essential tremor [5].
Dystonic spasms in the larynx are accompanied by incoordination of the vocal and vestibular sections; as a result, in addition to dystonic spasms of the vocal cords during phonation, excessive activity of the vestibular section of the larynx is observed, which is the essence of the functional mismatch of movements in laryngeal dystonia.
Laryngoscopy in all patients with a severe form of spasmodic dysphonia reveals significant tension in the vestibular part of the larynx - a decrease in its anteroposterior size, hypertrophy and increased tone of the vestibular folds. Sometimes you can see asymmetry of the larynx due to increased tone and hypertrophy of one of the vestibular folds. Characterized by increased motor activity of the entire vestibular part of the larynx: the vestibular folds are actively involved in phonation, and they involuntarily close, interrupting smooth speech.
In patients with mild voice impairment, the leading sign is trembling of the voice against the background of quiet, calm, intelligible speech. Tension and occasional stuttering appear only when the patient raises his voice. During laryngoscopy, the vocal cords look pale, their incomplete closure in the middle third and trembling during phonation are noted. There is a slight increase in the vestibular folds, which are involved in phonation, but their closure occurs extremely rarely or is not observed at all.
It has now been shown that hyperkinesis in laryngeal dystonia is not limited to the larynx, but extends to all parts of the vocal system (articulatory apparatus, larynx, diaphragm) and, in addition, is accompanied by mild motor impairment outside the vocal system [6].
Thus, spasmodic dysphonia is not a dysfunction of the larynx exclusively, since it is based on a violation of the central regulation of voice production and, as a consequence, functional mismatch or functional disintegration of all subordinate links of the voice production system.
Pathogenetic mechanism of spasmodic dysphonia
The severity of spasmodic dysphonia can range from mild to severe. Severe voice impairment is characterized by complaints of intermittency and trembling of the voice, severe involuntary spasms in the larynx during speech, and a feeling of fullness in the chest. At the same time, one gets the impression that speech requires great effort from the patient. It is accompanied by tension in a number of muscle groups and straining. By talking, patients help themselves with their whole body. A grimace of effort appears on their face with wrinkling of the forehead, nose, and squinting of their eyes. Often during a conversation, facial hypermia, congestion of the neck veins are noted, sweat appears on the face, head, and torso. Speech has the appearance of a rough, hoarse, intermittent whisper, unintelligible and laconic.
With the adduction type of spasmodic dysphonia, a strained, tense, unnatural voice is noted. This occurs as a result of the vocal cords closing too close. With the abduction type of spastic dysphonia, the ligaments move away from each other, as a result of which the voice becomes silent and airy. In both cases, the manifestations of this pathology can change every day. People with spasmodic dysophnia report difficulty communicating with strangers or speaking in public. Communication on the phone is especially difficult.
Like many types of dystonia, manifestations of spasmodic dysphonia are associated, for the most part, with a certain type of activity. Other functions of the larynx, such as breathing, are not impaired. Sometimes the voice may be normal when singing or laughing, but during normal conversation its pathology appears. This property of this disease, combined with changes in the characteristics of the voice during emotional stress, sometimes leads to a misconception about the mental causes of its occurrence. However, spasmodic dysphonia is not a psychiatric or psychological disease [7].
Methods of treatment and correction for spasmodic dysphonia
Previously, the only treatment for spasmodic dysphonia was voice therapy, which produced relatively little results. In 1976, Dedeaux proposed a rather radical means of opening one of the recurrent laryngeal nerves in an attempt to break the cycle of excessive vocal fold adduction. Now, reversal laryngeal nerve section has become the predominant treatment for spasmodic dysphonia, and more than 75% of patients report significant voice improvement after this surgery [2]. Approximately 12% of patients treated with recurrent laryngeal nerve exposure experience a recurrence of spasmodic dysphonia. As a rule, these patients before surgery were classified as having the most severe form of spasmodic dysphonia [2]. Interestingly, relapse of spasmodic dysphonia in such patients was associated with reapproximation of the vocal cords and was alleviated by removing a thin layer from the vocal cords with a CO2 laser. Because the left nerve is longer and has a higher incidence of idiopathic palsy, it is recommended, if necessary, to open the recurrent laryngeal nerve by cutting the left nerve.
Unfortunately, there is currently no complete cure for spasmodic dysphonia. Treatment, however, can reduce the manifestations of this pathology.
The most popular treatment for spasmodic dysphonia currently is injection of botulinum toxin into the muscles of the vocal cords.
[7]. Botulinum toxin is a waste product of Clostridium botulinum. As you know, botulism is a serious infectious disease that manifests itself with neurological disorders. Botulinum toxin affects nerve fibers, causing them to stop transmitting nerve impulses. This leads to paralysis of the muscles they innervate. The same principle of action of botulinum toxin is based on its use in the treatment of spasmodic dysphonia. The toxin relaxes the muscles that cause excessive contraction of the vocal cords. Neither medication nor psychotherapy or voice therapy alone can control the symptoms of spasmodic dysphonia.
Botulinum toxin has been used in medicine since 1984. The basis of its use, as already mentioned, is muscle relaxation. In the case of adduction spasmodic dysphonia, these are the muscles that close the vocal folds. In the case of abduction spasmodic dysphonia, these are the muscles that push the vocal cords apart. An injection into the muscles of the vocal folds is carried out through the skin in the neck area. The procedure is usually performed on an outpatient basis and after the procedure the patient can safely go home. In the case of adductive spasmodic dysphonia, after an injection into the muscles, the voice may be aspirated and whispering for some time; sometimes, when taking liquid, the patient may choke or cough. If this side effect is too pronounced or lasts more than 7–10 days, then the injected toxin is corrected. In the case of abduction spasmodic dysphonia, when the muscles that open the vocal cords are excessively relaxed, breathing difficulties may occur. It is worth noting that in the case of this type of spasmodic dysphonia, it is somewhat more difficult to avoid complications.
If treatment of spasmodic dysphonia with botulinum toxin injections is ineffective, surgical intervention is used on the nerves that approach the larynx (their dissection or destruction). This method has good results, however, in the case of severe spasmodic dysphonia associated with brain pathology, the disease may recur after several months or years.
It is also important to note that with spastic dysphonia, the voice is usually not restored on its own, that is, without special phonopedic classes. As a result of certain vocal efforts, surgical and drug treatment, a person develops a loud, modulated voice. The quality of this voice depends on the full functioning of the true vocal folds, the degree of their participation in the process of phonation, the activity of the resonators and the respiratory apparatus.
Restoring voice quality with spasmodic dysphonia is a very difficult task, sometimes more difficult than evoking the sound of the voice. This is due to the fact that the patient develops a pathological reflex of voice formation. In addition, such a voice is usually formed with the compensatory participation of false vocal folds in the process of phonation (false vocal folds), resulting in a hoarse, guttural tone. Therefore, the phonopedist is faced with the task of improving the sound quality of the voice, activating the normal activity of the true vocal folds, the oropharyngeal resonator and the respiratory system.
Activation of the vocal folds requires special exercises: moaning or imitation of mooing, imitation of a pigeon coo, coughing, pronouncing the vowel a
on a hard attack, massage of the larynx, as well as speaking into a mask [3].
Tactile-vibration, visual and auditory control help to tune the voice to sonority, composure and flight. In the process of simulating mooing, the search for the correct vocal delivery helps to obtain the sound of the voice in the “resonator position,” i.e., in the oral position, with minimal tension in the muscles of the larynx and abdominal muscles [1]. At the same time, the quality of the sounding voice improves (its volume and sonority) due to the inclusion of deformed true vocal folds in phonation to the detriment of tense and overly activated false vocal folds. Next, the sound m
is combined with vowels in forward and backward syllables, first in the middle register of the voice. Then the voice rises and falls, strengthens and weakens when pronouncing vowels, consonants, and syllables. In this case, the phonopedist draws the patient’s attention to the correct formation of sounds in the oropharyngeal cavity.
Conclusion
So, as we found out, laryngeal dysphonia is a complex organic disorder that requires an integrated approach not only to diagnosis, but also to the treatment and correction work itself. When correcting spasmodic dysphonia, the longest period is the development of height, strength, timbre of the voice, staging of the singing voice and improvement of the melodic and intonation side of speech. This is due to the fact that an established pathological conditioned reflex connection requires a long and painstaking restructuring. It is advisable to begin phonopedic work for spastic dysphonia after all medications, physiotherapeutic or surgical interventions. In this case, constant monitoring of the quality of the sounding voice is necessary, and this is possible only if the patient is conscious of his defect.
Literature:
1. Almazova E. S. Speech therapy work on voice restoration in children, M. - 2007
2. Diseases of otorhinolaryngology. Current section. Voice disorders, M. - 2005
3. Lavrova E. V. Speech therapy. Fundamentals of phonopedia, M. - 2007
4.
ENT - Otolaryngology - Оtolaryngology.ru
—
2007
5.
V. S. Myakotnykh. Paroxysmal neuromuscular syndromes. State Educational Institution of Higher Professional Education "UGMA FA for Health and Social Development". 2010
6. Corrective phonopedic work in patients with spasmodic dysphonia: Method. recommendations / Ministry of Health of the RSFSR; [Compiled by O. S. Orlova and others], M. Ministry of Health of the RSFSR 1984
7. https://medicalplanet.su/neurology/408.html
Psychogenic dysphonia
With psychogenic dysphonia, there is a deterioration in the voice up to its loss due to some psychogenic reasons. Usually, when exposed to a stress factor, a person begins to become very worried and worried, after which problems with speech appear. In terms of symptoms, they resemble hyperfunctional dysphonia with unstable speech and typical squeezing.
In the psychogenic form of the disease, a mandatory consultation with a psychologist or psychiatrist is required. Doctors set themselves the goal of stopping and, if possible, eliminating a negative reaction to the stimulus. A speech therapist will help with restoring normal speech and returning to normal communication.
Speech specialists are engaged in the diagnosis and professional correction of speech disorders. We will determine the cause of dysphonia and help restore speech without drugs or hypnosis.
Main manifestations
An increase or decrease in tone in the vocal folds, incomplete closure of the glottis, tonic muscle spasm of the larynx and convulsive approach of tense vocal folds, discoordination in the work of the external and internal muscles of the larynx, vibrating voice, confusion of speech breathing, discomfort in the throat.
The heterogeneity of forms of voice disorders determines the diversity of their clinical manifestations. The differences between them are due primarily to the nature of the disorder (organic or functional, congenital or acquired); location and size of the lesion. The specifics of voice dysfunction in each form of Dysphonia (hypotonic, hypertonic, hypo-hypertonic, mutational, spastic) are also determined by: duration of the disorder (short-term or persistent changes), degree of severity (severe, moderate, mild), stage of the disease (early or late recovery ), pathogenetic mechanisms (nature of the disorder).
Treatment
Treatment should be comprehensive and include both local, which consists of sanitizing foci of infection, and general somatic treatment. It is aimed at increasing the endurance of the voice-producing apparatus and developing stable phonation skills. Treatment without the use of medications includes:
- Carrying out phonopedia - pedagogical education of correct voice production;
- Breathing and articular gymnastics;
- Acupuncture and physiotherapy, which include procedures such as dynamic currents, electrophoresis on the larynx area, amplipulse (pulse current treatment)
- Psychotherapy;
- Massage of the collar area.
During drug therapy, stimulant drugs are prescribed. In cases of severe and persistent hypophonia, implantation therapy is used.
Etiology
The causes of voice loss in children are as follows:
- constant imitation of car or steam locomotive whistles;
- overstrain of the vocal cords during screaming;
- hypertrophy of adenoid tissue;
- imitation of the voices of fairy-tale characters.
Factors contributing to the development of functional dysphonia:
- laryngitis in acute form, especially recurring;
- systematic overstrain of the vocal cords;
- disruption of the innervation of the muscular structures of the larynx in various pathologies of the nervous system.
Factors in the development of organic dysphonia:
- tumor-like formations in the lung tissues, which can put pressure on the laryngeal nerve fiber;
- papillomas;
- laryngitis that has become chronic;
- traumatization of the larynx during surgical intervention in this area;
- benign and malignant laryngeal tumors.
Causes and course of the disease
One of the reasons for the occurrence of functional dysphonia is considered to be structural features of the vocal apparatus, which can be anatomical, congenital and constitutional. In addition, this disease can occur with voice overexertion, asthenic syndrome (chronic fatigue) of various etiologies, as a complication after respiratory diseases, under the influence of psychotraumatic influences. The following factors can have a serious impact on the occurrence of such a disorder:
- Surgical operations on the larynx;
- Forced long silence;
- Hormonal disorders;
- Parkinson's disease;
- Traumatic brain injuries;
- Disturbances in cerebral circulation;
- Myasthenia gravis (muscle weakness).
Functional dysphonia is a reversible disorder. However, with a long course, it can cause the development of atrophic laryngitis, the formation of pseudofold phonation, which sometimes causes hypertrophic (pathological enlargement) changes in the vestibular folds. Hyperkinetic (or spastic, that is, caused by voice overexertion) dysphonia often leads to persistent disruption of microcirculation of the vocal folds, which causes ulcers, polyps, nodules and other pathologies in the larynx.
The causes of spasmodic dysphonia, when the vocal folds move involuntarily, are currently not fully understood.
Mutational dysphonia
Mutational dysphonia usually occurs in boys during puberty, when the voice “breaks” and becomes rougher. The reason is various functional changes in the speech apparatus due to hormonal changes. If these processes occur significantly and disrupt normal speech, it is recommended to consult a specialist.
A speech therapist will help the child quickly adapt to such changes; with the help of training, speech can be maintained within acceptable limits. If due to dysphonia there is a loss of voice or its quality is impaired, a specialist will help you quickly rehabilitate in a difficult situation.
Hypotonic dysphonia
The word “hypotonicity” means weak tone, in this case, of the muscles of the larynx. In simple terms, the muscles of the speech apparatus contract with insufficient strength, which leads to a weak or hoarse voice, speech becomes illegible and poorly understood.
The cause of hypotonic dysphonia is organic in nature; it develops when the muscles of the larynx themselves or the nerves that control the contraction of these muscles are damaged. Before treatment, an examination by an otolaryngologist and a neurologist is required to exclude pathology. Only with a comprehensive diagnosis can the exact cause of the disease be determined.
Hypertonic dysphonia
This form of dysphonia develops due to overstrain of the vocal muscles, which are responsible for generating sounds. Due to the high tone, tension in the neck muscles is noted, the phonation is sharp, and pronounced hoarseness is observed. Hypertonic dysphonia in severe cases may be accompanied by shortness of breath with dry wheezing due to narrowing of the glottis.
Sometimes patients need urgent help - the earlier treatment is started, the easier and faster it is to restore a normal voice. Muscle contraction also develops with certain diseases of the larynx or with psycho-emotional stress.