Reasons for appearance
With aphasia, certain areas of the brain that are responsible for speech are damaged. Most often this occurs against the background of a stroke, traumatic brain injury, or vascular aneurysm. Adolescents and young adults are at risk of developing the disease.
Childhood aphasia occurs due to the following reasons:
- brain tumors;
- injuries;
- severe infectious disease.
This is a severe disorder that affects all types of speech activity. The severity of the problem depends on the location of the lesion, its size, and impaired functions.
What matters is the person’s reaction to the defect and its awareness. The degree of development of skills, such as reading, before the appearance of the defect is taken into account.
Aphasia should not be confused with other problems: alalia, dysarthria. The child develops a number of specific symptoms. The cause of the violation is always organic in nature.
Aphasia rarely occurs in children - about 10% of cases occur in preschool and school age. The rest of the patients are people over 18 years of age.
Due to a sedentary lifestyle and worsening crime situation, strokes and traumatic brain injuries are significantly younger. The number of tumor diseases has increased. Therefore, the development of speech restoration methods is relevant.
Children are more often diagnosed with motor and sensory aphasia. In adults, the forms of the disease are varied.
Features of aphasic disorders in children and adolescents with traumatic brain injury
Traumatic brain injuries (TBI) account for 40% of all traumatic injuries in humans. The consequences and complications of TBI are very diverse. The most common consequence of TBI is aphasia (systemic disorders of speech function) or dysarthria, which are often combined with pathology of other higher mental functions (HMF). A special problem in terms of theoretical study and its practical implementation is aphasia in children, including aphasia of traumatic etiology.
Descriptions of aphasia in children are available in the works of a number of authors (S.Yu. Benilova, T.G. Vizel, Yu.A. Mikadze, A.Yu. Obukhovskaya, A.V. Semenovich, E.G. Simernitskaya, N.N. Traugott, M. G. Khrakovskaya, L. S. Tsvetkova, etc.). Researchers note that the clinical picture of childhood aphasia has both similarities and differences with aphasia in adults.
The similarities are as follows. In both children and adults, aphasia occurs due to the same etiological factors. The most common injury in children is traumatic brain injury. Aneurysm ruptures occur less frequently, as do tumors; even less common are strokes (in contrast, in adults strokes occupy a leading place). The similarity between children's and adult aphasias also lies in the fact that in both groups there is a disintegration of already formed speech. Hence the identity of many symptoms of aphasia in children and adults, as well as the presence in the acute period of the disease of a significant amount of neurodynamic disorders that obscure the main syndrome.
The differences between childhood and adult aphasia relate, first of all, to the degree of persistence of speech pathological symptoms. Speech disorders in children are less persistent than in adults, are observed more often in the acute period of the disease and have a relatively rapid reverse development. As is known, this is associated with the high plasticity of the child’s brain, in which the functional activity of interzonal connections, rarely mentioned in the literature, is important.
Despite the existing developments, the problem of aphasia in children and adolescents is still insufficiently studied, especially with regard to the processes of correctional and restorative education.
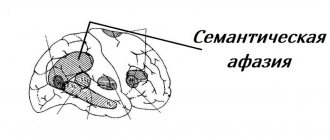
The most common and recognized is the classification of aphasia by A.R. Luria, which includes: afferent motor, efferent motor, dynamic, sensory (acoustic-gnostic), acoustic-mnestic, semantic. Semantic aphasia is most rarely detected in children and adolescents due to the immaturity of the tertiary zone of overlap of the cerebral cortex (TPO zone) in childhood. The diagnosis of semantic aphasia is valid after the age of 12-13 years.
Unfortunately, in the acute period it is not always possible to conduct a full speech therapy examination due to the severity of the patients’ condition or their increased exhaustion. In children, these features of the acute period of the disease are expressed to an even greater extent due to the immaturity of the HMF, as well as the emotional-volitional sphere. This determines that in most cases the speech therapist conducts a blitz examination, aimed primarily at identifying speech disorders, using various modified diagnostic scales. The following is assessed: the state of the pronunciation side of speech, understanding of addressed speech, the level of the state of oral speech, reading, writing, oral and articulatory praxis, and not only a qualitative analysis is carried out, but also a quantitative assessment in points, for a visual representation of the dynamics of recovery. The degree of complexity of the diagnostic material varies depending on the age of the child and the level of development of his speech and other HMF. For some, in particular preschoolers, it is advisable to select simplified diagnostic techniques similar to standard speech therapy examinations of children with ODD. The observation method is also used. The diagnostic procedure is preceded by the collection of anamnestic information about the physical and psycho-speech development of the child. Particular attention is paid to the extent to which he spoke before the injury. In this case, it is necessary to take into account the age parameters of the maturation of HMF.
Diagnostics, depending on the patient’s condition, can take from 10 to 40 minutes. Based on the diagnostic results, the speech therapist determines the form of speech disorders in the patient, the degree of their severity (mild, moderate, severe) and the leading defect; evaluates the characteristics of neurodynamic processes.
According to Simernitskaya E.G. the clinical picture of speech disorders in children becomes similar to aphasia in adults from the age of 6 years. Before this age, speech disorders are similar to alalia, although the child’s speech development before the traumatic impact on the brain could be normal; after a TBI, speech is impaired, but the diagnosis of “aphasia” is made only when the child’s speech is already formed. In the case where the child had a history of speech development delays like alalia before the TBI, after the injury the clinical picture of speech worsens. Experience also shows that speech impairments in preschoolers are more difficult to recover. According to parents, emotional and behavioral disorders appear or worsen: children become more capricious, and even more often aggressive. At the same time, it has been established that all children have higher compensatory capabilities than adult patients. The plasticity of the children's brain allows them to overcome disorders in a shorter time and achieve positive dynamics earlier. Currently, rehabilitation departments often receive patients who are bilingual and whose speech communication is impaired in both their native and non-native languages. Care for such patients should be provided either in their native language or in both languages. According to our observations, assistance in a language other than one’s native language is not sufficient to correct speech disorders.
Restoring speech function in any form of aphasia requires a systematic approach, i.e. implies the normalization of all disturbed systems of speech function, as well as the non-speech HMFs that are basic to it. It has been established that the earlier speech therapy work is started, the better its final result, so rehabilitation begins in the first days, when even the most minimal contact with the child becomes possible. The principles and techniques of working with various forms of aphasia are described in the literature. With adolescents, techniques and methods developed for adult patients are used (it is possible to use all benefits for the recovery of aphasic disorders). When working with preschoolers, preference is given to gaming techniques: games, physical exercises, finger exercises, elements of dramatization (fairy tales, skits using toys), logorhythmics.
Purpose of the study: to study the characteristics and dynamics of aphasia in children and adolescents with severe and moderate traumatic brain injury.
Materials and methods of research.
The study was conducted on the basis of the Scientific Institute of Emergency Pediatric Surgery and Traumatology (Research Institute of Pediatric Surgery and Traumatology). 20 children with traumatic etiology of aphasia were examined. The children were distributed by age and gender as follows: from 4 to 17 years old - 5 girls and 15 boys, among them 4 preschool children.
The following methods were used:
- Diagnosis of the state of speech function and other HMFs using a complex neuropsychological technique using diagnostic schemes by A.R. Luria, L.S. Tsvetkova, V.M. Shklovsky and T.G. Wiesel, including non-speech and speech scales.
- Corrective and remedial training.
Results.
In all children and adolescents in the most acute period, predominantly gross motor aphasia and gross sensory aphasia were noted, which subsequently manifested themselves in different clinical pictures. Among them, complex motor aphasia of varying degrees of severity predominated (in 17 children - 85% of the total number studied). The remaining children had: 1) acoustic-mnestic aphasia (in 12 children - 60%), the peculiarity of which was that it most often manifested itself as part of the amnestic syndrome; 2) dynamic aphasia (in 3 children - 15%), which usually manifested itself as part of the frontal syndrome. Two left-handed children (10%) had aphasia that was unrecognizable in the acute period.
The study confirmed and clarified the ideas that: 1) in children, just like in adults, neurodynamic disorders and disorders of executive functions (mostly in the levels of control and regulation) are clearly visible, which “noise” the true picture of a speech defect ; 2) in the process of rehabilitation training, neurodynamic disorders are leveled out faster than in adults. In addition, we found that neurodynamic difficulties go away somewhat faster than difficulties in executive functions.
The next result is the statement that gross sensorimotor aphasia regressed more quickly in children, especially its sensory component. Among the more persistent disorders were motor (with a predominance of the efferent component), as well as acoustic-mnestic disorders. It was also found that all children with TBI had amnestic disorders, mainly in the auditory-speech modality. All children, regardless of the form of aphasia, showed a violation of the nominative function, and the updating of the predicative vocabulary was carried out much better than the nominative one - even in children with motor aphasia.
Written speech and sound-letter analysis suffered in all children, regardless of age and form of aphasia. This also applies to the inferiority of dynamic praxis (in the form of deautomation of praxic actions). Disturbances in kinesthetic hand and finger praxis were less pronounced. Children with dynamic aphasia, like adults, showed significant impairments in speech communication.
In terms of recovery, preschool children, as well as children of primary and secondary school age, showed high positive dynamics in the restoration of speech and other HMF; In children of high school age, the symptoms of aphasia were similar to the dynamics of regression of aphasia in adults. This concerns not only the specific manifestations of aphasia, but also the well-known fact that serious difficulties arise in communication with others and socialization in general.
An analysis of the characteristics of the restoration of speech function in patients showed that the optimal teaching tactic is to follow its phased approach. At the early stages, the task was set to include involuntary, automated levels of speech activity. At subsequent stages of the disease, correctional and restorative training used restructuring techniques. This once again demonstrates: a) the compensatory activity of brain mechanisms in the early postmorbid stages due to vicariate reserves, as well as the inclusion of interzonal connections in compensatory processes; b) the need to search for brain mechanisms to bypass the primary defect in more distant periods of the disease.
Summarizing the results of the study, we can conclude that they basically confirmed the existing ideas about the features of the course of childhood aphasia, their similarities and differences with the features of the course of aphasia in adults. We regard the new data we have received on:
- quantitative and age distribution of forms of aphasia in children;
- patterns in the severity of individual symptoms;
- greater activity of interzonal connections in children than in adults;
- compliance with stages in rehabilitation training;
- methodological content of each of the recovery stages.
Let us give a clinical example from speech therapy practice.
Boy, Luke (4 years old).
The boy was admitted to the rehabilitation department with a diagnosis of consequences of traumatic brain injury (moderate brain contusion, comminuted fracture of the left parietal bone).
In the child's speech status, pronounced difficulties were detected, in the motor sphere - right-sided hemiparesis (more in the hand). In the emotional sphere, the child showed increased lability, fatigue, exhaustion, fluctuations in capabilities, and inactivity. At home, according to his parents, after the injury, the boy began to be capricious more often, cry, refuse to do many things that he had previously done with pleasure (he began to play less, got more tired, could scream if he didn’t like something, due to hemiparesis he could not used his right hand when performing everyday activities). In his premorbid status, Luka had well-developed speech in accordance with the age norm; he is a very active and inquisitive boy, right-handed (his relatives are also right-handed).
Objectively during examination: Luka in the situation of examination has adequate behavior, is contactable, criticism is reduced. Inertia, exhaustion, inactivity, an increase in the latent period, and fluctuations in capabilities are noted. Complaints from the mother about speech disorders, slowness in all types of activities.
Swallowing was preserved, chewing was normal. Violations of the muscle tone of the organs of articulation are revealed. The face is hypomimic. Tongue - dystonia. The voice is dull, poorly modulated. Speech exhalation is shortened. Salivation is moderate. Sound pronunciation - replacement of some sounds (as a variant of dysontogenesis in the form of erased dysarthria, as well as a phenomenon of afferent apraxia). Speech intelligibility in the speech stream is slightly reduced. The rate of speech is slow, the rhythm is disturbed.
Impressive speech. Speech understanding is preserved. Display of objects is difficult and confusing in places. The perception of extended speech is somewhat slow.
Expressive speech. Own speech is possible, but difficult and meager. Speech activity is reduced. According to the mother, before the injury he had phrasal speech, the child loved to perform various developmental tasks. Difficulties in organizing a monologue utterance, perseveration (repetitions of sounds, syllables and simple words), agrammatisms, permutations, and rare paraphasias are identified. Repetition of words and phrases - with rearrangements of sounds and syllables, perseverations, omissions of sounds. Naming is possible. Responses are often latent. Writing a story is difficult. Non-verbal tasks (with the help of picture material) are carried out well.
Speech therapy status: motor alalia, dysarthria, neurodynamic disorders.
Remedial training program:
- Correction of phrasal speech.
- Correction of the pronunciation side of speech, voice characteristics.
- Development of phonemic analysis.
After a course of rehabilitation training in the rehabilitation department, Luka’s speech status showed a pronounced positive trend. Luka began to use his right hand more actively (more often he began to pick up objects and pictures in his right hand in class), the neuropsychologist recommended that he develop fine motor skills at home and remind the boy to include his right hand in activities (if he is capricious, do not insist). The boy became calmer, emotional lability and exhaustion decreased (both at home and in class), active performance increased, Luka began to ask less often “will class end soon?”, and became less distracted. Face - facial expressions have become more animated. The performance of voluntary articulatory movements has improved, however, pathological synkinesis during tongue movements remains. The strength of the voice increased, the modulations became more pronounced. The voice became more sonorous. Speech active exhalation became smoother and longer. Salivation is moderate. In the speech stream, speech intelligibility improved. Sound pronunciation remains blurred, complex words are pronounced at a slow pace, with rearrangements and replacements of sounds. The sound “l” is inserted, although in speech the hard sound is still replaced by a soft one (“l” - “l”). The rate of speech became faster, closer to normal, the rhythm was maintained.
Impressive speech. Speech understanding is preserved. I became better able to retain presented elements in my auditory-verbal memory.
Expressive speech. Your own speech is possible, the phrase has become more developed, more words have been updated. Perseverations began to be observed less frequently, agrammatisms (characteristic of efferent apraxia), rearrangements of sounds and syllables, and rare paraphasias were noted.
Upon discharge, the boy showed positive changes in all areas of activity and, in particular, in speech. To further restore the boy’s speech function, the parents were recommended to continue speech therapy classes at their place of residence and in rehabilitation departments. This is extremely important, given the fact that Luke’s speech was not yet fully formed, but was in a stage of development.
Thus, all of the above and the example given leave no doubt that the development of the problems of aphasia in children, including traumatic etiology, is far from complete. It is necessary to further study it, and above all, to search for special methods and techniques of restorative training that would help more effectively and efficiently overcome the aphasic disorders that children have.
Motor aphasia
Occurs in 90% of cases and occurs when the speech motor center of the brain is damaged. With this pathology, a person does not speak or reproduces abrupt phrases.
With motor aphasia, the patient understands the spoken speech, but is not able to reproduce it himself.
He is not able to repeat sounds, syllables, words, simple phrases. Sometimes he spontaneously says something - common expressions, everyday sentences, random syllables. Spontaneous speech is impossible.
Children experience a partial or complete breakdown of written speech; reading suffers more than writing. Attempts to read a text out loud are accompanied by paralexia - incorrect recognition of letters, inability to combine them into syllables.
In the process of speech therapy research, it was discovered that with motor aphasia, children are able to correctly write down a digital sequence and add a first and last name from a split alphabet.
Personal characteristics:
- self-criticism;
- feeling of helplessness;
- awareness of the defect;
- uncertainty.
In severe cases, the combination of these problems leads to depression. It has a bad effect on children's development.
Symptoms
The clinical picture depends on the form of dysphasia.
- Acoustic-gnostic. Occurs after damage to the temporal cortex of the dominant hemisphere. Characterized by impaired speech understanding. The child hears dialogue not as a set of outlined words, but as a collection of meaningless sounds. Often combined with impairments in counting, reading and writing.
- Amnestic form. Occurs when the posterior region of the temporal lobe is affected. Amnestic dysphasia is based on a violation of auditory and speech memory and a violation of the nominative function, when the baby forgets the name of an object or phenomenon and tries to describe it in words.
- Afferent motor dysphasia. Occurs after damage to the inferior frontal gyrus behind the dominant hemisphere. It is based on a violation of the innervation of the muscles responsible for articulation. Speech becomes difficult to understand and, with severe impairments, becomes inarticulate.
- Efferent motor aphasia. Occurs after damage to the posterior region of the frontal region of the dominant hemisphere. Efferent dysphasia is different in that it is difficult for him to form speech and correctly build its structure and sequence.
- Dynamic form. Diagnosed in adolescents. Occurs when the posterior structures of the frontal lobe are damaged. Symptoms are increased speech production and the predominance of speech patterns in it. This is manifested by the fact that the baby does not say anything other than stereotypical everyday phrases, and answers questions as briefly as possible - “yes” or “no.”
Sensory aphasia
The etiology of appearance is that the center of the brain responsible for speech perception is affected. The patient has excellent hearing, but he does not understand anything he hears. Similar feelings arise in people who hear foreign speech.
Experts distinguish two degrees of severity. When severe, a person does not perceive his own or someone else’s speech. If it is mild, he does not understand certain semantic structures. In the absence of work to eliminate the defect, the number of recognizable words decreases.
This form is rare in children. Secondary violations:
- low degree of concentration;
- intellectual disabilities;
- lack of need for social interaction.
In the process of restoration work, attention is paid to developing contact and stimulating positive emotions. The correction takes a long time and requires a lot of effort from specialists and parents.
With sensory aphasia, the child is talkative, uses speech, but does not control it. Despite the verbosity, the flow of speech is meaningless.
Acoustic-mnestic aphasia
Articulation
Oral and articulatory praxis (movements) without disturbances.
Spontaneous speech
Spontaneous speech is characterized by difficulties in selecting the words necessary to organize a statement and is represented by short phrases, varied in lexical and grammatical structure. At the same time, there are quite frequent verbal paraphasias (replacement of some words with others that are close in meaning) and pauses due to the characteristic difficulties of finding the right word. In long words with a complex sound structure, there are distortions in the sequence of the sound scale that makes up the word: rearrangements, omissions, additions of sounds and words as a result of anticipation, weakness of acoustic traces. It is especially difficult for the patient to produce low-frequency words.
Speech automatisms
Easily cope with all types of direct automated speech. Counting backwards, listing the days of the week, months in reverse order is accompanied by perseverations, exhaustion of attention, slipping into the direct order of listing, etc.
Repeated speech
Repeated speech as a function does not suffer, but errors occur due to insufficient retention of the perceived text. Words and phrases that are accessible for direct perception and repetition turn out to be forgotten, “erased” after the introduction of some kind of interference (pause, question, counting, etc.).
Dialogue speech
Dialogical speech appears to be impaired.
Naming
There are difficulties in naming, mainly objects. The basis is a deficiency in the field of visual representations. Difficulties in updating proper names and numbers are often expressed.
Phrase based on the plot picture
The possibilities of constructing a phrase based on a plot picture correspond to the possibilities of oral speech.
Retelling texts
Retelling is difficult in a significant way. Its quality directly depends on the length of the story and the complexity of the plot, i.e. The main obstacle is the difficulty of retaining fragments of text.
Speech understanding
Understanding short speech structures is usually accessible. When perceiving more detailed texts, errors in comprehension are revealed. Patients begin to worry, ask again, ask to speak more slowly. Displaying objects and body parts by individual names is available. When presented with a series of names, alienation of the meaning of the word occurs. No primary phonemic hearing disorders were detected.
Volume of auditory-speech memory
The volume of auditory-speech memory is insufficient to retain a speech sequence even of 3 or more elements - vowel sounds or words.
Read function status
Reading as a function does not suffer. Comprehension is closely dependent on the length of the text being read.
Writing function status
The state of the writing function “leads” oral speech, regardless of the severity of the defect. The sound-letter analysis of the composition of a word does not suffer primarily, however, in writing from dictation there are errors associated with difficulties in retaining a text perceived by ear: omissions of words, verbal paraphasia (replacement of sounds and syllables).
Diagnosis differentiation
Determining the exact speech disorder is not always easy. In speech therapy, there are different diseases that have certain characteristics. With dysarthria, the subcortical structures of the brain are affected, and problems with pronunciation arise. In aphasia, gross motor disturbances arise due to damage to areas of the cortex. Dysarthria is characterized by limited articulatory apparatus, which is observed in all situations.
The symptoms are similar to alalia, but these are two different diagnoses. Aphasia is the breakdown of speech that has begun to form normally. The child pronounces the sounds of early ontogenesis, constructs simple phrases, and accumulates a vocabulary. With alalia this does not happen - there are no words, syllables, sometimes only simple onomatopoeia (“ma”, “bibi”).
With aphasia, a normal level of physical hearing is noted. The child reacts to stimuli and extracts speech sounds from the environment.
If there are mental disorders - developmental delay, mental retardation, autism - aphasia is not diagnosed. Against this background, secondary defects may develop, but they do not lead to a similar problem.
Diagnostic methods
Before you begin to fix the problem, you need to correctly determine the cause of the problem. This will allow you to choose the direction of restoration work and carry out treatment. Examinations are prescribed by a neurologist.
An MRI (magnetic resonance imaging) or computed tomography scan can help determine the location of the problem. Knowing which areas of the cerebral cortex are damaged will help determine the work needed.
In the sensory form, Wernicke's area is affected; in the motor form, Broca's area is affected.
It is advisable to conduct an ultrasound of the brain vessels - this will reveal circulatory disorders.
A psychologist assesses the state of higher mental functions (HMF):
- memory;
- thinking;
- attention.
This is an important stage of the examination, as it makes it possible to determine secondary disorders. With visual agnosia, the patient sees an object, but is unable to recognize it. That is, he describes the chair and its functions, but cannot name it.
The speech therapist conducts pedagogical diagnostics. It is aimed at studying general, fine motor skills, and organs of articulation. With the motor form, apraxia appears - the inability to perform a series of movements.
During a conversation, shifts in syllables occur. In severe cases, the style of speech, that is, the patient does not use verbs, prepositions, his phrases are short and chopped off.
Written language diagnostics is carried out in school-age children. A text is given to copy, one sample with written letters, the other with printed letters. The third test is taking dictation. A reading test is required.
In a severe form of motor aphasia, a child is able to write down a word only if it is clearly pronounced in syllables - this is a manifestation of agraphia. With sensory input, the patient easily copies the text from the sample and reads it. But without auditory control it does not always sound crisp and clear.
First aid is provided in hospitals, where children are checked by a council of specialists. In early forms of aphasia, it is difficult to make a prognosis, since much depends on the degree of damage, the beginning of assistance, and the qualifications of specialists.
Speech examination “Diagnostics of aphasia”
EXAMINATION OF DISTURBED
HIGHER CORTICAL FUNCTIONS
Like any speech therapy examination, examination of speech in aphasia begins with a preliminary conversation that allows establishing contact with the patient, assessing:
1) speech capabilities,
2) preservation of consciousness,
3) criticality,
4) orientation in the environment, in location, in time.
The patient is asked questions about his well-being, the time of year, the date of his illness, his educational level, specialty, marital status, the presence of left-handers in the family, etc. are found out.
Determining the presence of left-handedness
:
1) interlacing of fingers.
2) crossing arms over the chest (for a left-handed person, the left hand lies on top);
3) aiming when simulating archery.
4) along the venous network (brighter on the leading arm)
Examination of non-speech praxis and gnosis
is carried out using non-speech examination methods, which make it possible to identify the integrity or impairment of the parietal lobe, posterior frontal and premotor parts of the occipital regions.
Dynamic Praxis Research
is carried out by patients performing imitation, and then following an oral task, tests
for switching from one movement to another.
The patient holds his hands on the table and simultaneously changes their position.
In the presence of dynamic premotor apraxia,
the patient begins to repeat the same movement with one hand or another, loses rhythm (
reciprocal test)
. The “fist-rib-palm” test is designed to study the integrity of the movement plan
.
In the presence of premotor apraxia,
the patient does not maintain the plan of movements, skips and repeats individual movements.
The presence of dynamic apraxia
indicates the presence of a lesion in the premotor and posterior frontal regions, and in some cases in the subcortical regions of the cerebral cortex.
Spatial Praxis Survey
allows us to judge the safety or disruption of complex simultaneous syntheses. In patients with extensive damage to the upper nonparietal parts of the brain
There may be signs of spatial disorientation in everyday life. Patients cannot find their room, cannot dress properly, etc. The following tests are offered:
- Head's samples. The patient is asked to imitate the following movements together with the speech therapist: bring the index finger to the chin, turn the hand palm up and fingers away from the chin, place the left palm perpendicular to the chin, place the palm perpendicular to the other palm, etc. The patient’s orientation in the left and right side of the body.
- Copying by the patient various figures made from matches, folding them upside down, the KOOS technique. In addition, the patient’s reproduction of symbolic movements is examined: the patient is asked to wag his finger, beckon someone to come to him, clap his hands, depict cutting paper, cutting bread, etc.
- Test with a clock and a geographical map. The patient is asked to determine the time on a drawn clock without numbers in the direction of the arrows; draw arrows conveying this or that time; find seas, cities, countries on the map; mark the location of north and south, east and west on the axes crossed perpendicularly; draw the contours of the Black Sea, etc.
4. The patient’s orientation is checked among letters written correctly, mirror and horizontally on the line.
Difficulties in performing these tests are typical for patients with afferent and semantic aphasia
, i.e., with damage to the posterior inferior parietal parts of the brain.
When the premotor and posterior frontal
parts of the cerebral cortex are damaged, inertia and impaired planning of actions and movements are revealed when performing a series of these tasks.
Rhythm evaluation and playback
The patient's ability to motor switch from one rhythmic pattern to another and the tendency to simplify the rhythmic pattern are checked. The speech therapist taps the rhythm on the table with a pencil, covering it with a sheet of paper, two or three beats at a time, in different series: two strong, two weak, two fast, one delayed, etc.
Patients who do not maintain a given rhythm, automatically add, repeat one group or series of beats, or add extra beats, repeating them due to perseveration, belong to the group with damage to the premotor and posterior frontal parts of the cerebral cortex. Patients with sensory aphasia
refuse to play rhythmic beats, stating: “There are a lot of them.”
Patients
correctly reproduce rhythmic patterns from auditory imitation, but cannot describe the nature of the rhythms.
Visual gnosis examination
carried out to distinguish speech disorders from naming difficulties with visual agnosia that occurs with damage to the tertiary parts of the occipital lobe and to clarify optical alexia that occurs with damage to the parietal parts on the left. The patient is asked to name or describe objects or their images. He is given simple, clear, contrasting object pictures, then similar in shape (ball, apple, globe, glasses, bicycle, etc.). Then they are replaced by single-color, contour, speckled (covered with small dots), crossed out with zigzag lines and contour images superimposed on each other. Patients with visual agnosia have difficulty recognizing and describing the functions of objects.
Letter recognition
written in different fonts is tested in well-speaking patients by naming them and showing them according to instructions. Patients with optical alexia have difficulty completing these tasks.
Oral and facial praxis examination
Violation of oral and facial praxis
often combined with a violation
of articulatory praxis
. Oral praxis includes non-speech movements of the oral apparatus, i.e. lips, tongue, cheeks.
The study consists of the following tests:
- the patient is verbally given instructions to open his mouth, stick out his tongue, lift it up, down, move it to the left, to the right, click his tongue, put his tongue behind his cheek, inflate his cheeks alternately and at the same time, stretch his lips forward, stretch his lips.
- The patient performs the same tasks by sightsolid imitation
.
- Next, according to the oral task and visual imitation, various symbolic movements
: blowing, imitation of spitting, whistling, imitation of gargling, coughing, reproducing a smile, raising eyebrows as a sign of surprise, winking, etc.
The patient performs all these tests in isolation, with pauses between tasks. Difficulties in performing these tasks in different localizations manifest themselves in different ways. For pseudobulbar dysarthria
profuse salivation, viscosity, incomplete movements, and changes in facial expressions appear.
With lower parietal lesions,
various chaotic searches arise and difficulties in giving the articulatory organs the appropriate positions.
Patients with oral, inferior parietal apraxia
cannot voluntarily depict the movement of a kiss or spit according to instructions, while these movements are preserved in everyday life.
Oral, inferior parietal apraxia
in some cases is observed in isolation, without speech disorders.
When the premotor and posterior frontal areas are damaged
, perseverations, repetitions of previous movements, and difficulties in performing serial tasks occur.
To test dynamic oral praxis, the patient is asked to perform a series of movements, such as blowing and flicking the tongue. Patients with premotor apraxia
perform individual movements well and get stuck on one of the movements included in a linearly organized series of movements due to perseveration.
At the same time, sometimes there is an illusion of the presence of simultaneous , constructive, spatial apraxia
with damage to the premotor parts of the cerebral cortex.
In case of extensive lesions of the frontal lobes,
due to severe inactivity and spontaneity, involuntary spitting and coughing are impaired, while the performance of these movements is relatively intact when stimulated.
Examination of speech functions
Examination of speech functions
covers
all types of impressive and expressive human speech activity,
this includes:
1) indicative examination of spontaneous speech
(during
a preliminary conversation with the patient)
. The speech therapist records the activity and volume of the patient’s speech production (when examining a speechless patient, the speech therapist notes whether he is active, whether he is trying to answer questions with the help of emboli, whether his speech is sufficiently colored with various intonation shades or whether he is indifferent).
2) examination of speech understanding.
Before proceeding with the examination of understanding, the speech therapist needs to make sure
that the patient’s hearing is intact
, and also find out how many times he has had cerebrovascular accidents and what they were accompanied by.
3) examination of phonemic hearing.
The patient is asked
to repeat close (oppositional) phonemes
: for example, on
b
, raise your hand, and on
p
, keep your hand on the table, then a series of syllables ba, pa, pa, ba, pa is given. Finally, phonemic awareness can be explored by showing appropriate syllables or words with opposition sounds (house-tom, barrel-kidney).
For severe acoustic-gnostic sensory aphasia
at an early stage after a stroke, patients do not distinguish even phonemes that are distant in sound, later - only phonemes that differ in one acoustic feature: voiced - unvoiced, hard - soft, whistling - hissing.
Phonemic hearing is secondarily impaired in gross afferent motor aphasia
due to a violation of kinesthetic afferentation.
Patients do not distinguish by hearing phonemes that are close in place and method of articulation (m - b - p, n - d - t - l) both in the perception of syllables and in the perception of words, however, phonemic hearing is
less impaired
in afferent motor than in acoustic-gnostic aphasia
.
With pronounced efferent motor aphasia
, perseverations occur during the study of phonemic hearing.
4) examination of
understanding meanings .
During the examination, the patient is asked to show objects surrounding him (table, chair, book, pencil, window, door, ceiling, steps, closet, etc.), to show parts of the face and body.
Difficulties in showing parts of the body and objects in the room are observed in all forms of aphasia: in sensory aphasia - due to impaired phonemic hearing and instability of auditory-verbal traces; with efferent - due to the presence of perseveration in hand movements; with afferent and semantic - with rapid presentation of words due to difficulties in orientation in space.
Hearing-verbal memory impairments
are identified by the patient repeating a series of words (two, three or more), for example, house - cat - forest, hand - window - fish, etc. Patients are given the task to repeat the sentence.
Apple and pear trees grew in the garden behind a high fence. Patients with acoustic-mnestic aphasia,
unable to retain the speech sequence, usually miss the second and third words;
with efferent
patients persist the first or second word, as well as words from previous tasks.
Another technique for examining auditory-verbal memory
is to find,
laid out in front of the patient or
Secondarily, mild auditory-verbal memory can be impaired when both the frontal lobes of the brain and the inferior parietal parts of the left hemisphere are damaged in right-handed people.
5) examination of understanding of simple sentences:
1) the patient’s understanding of simple and relatively complex instructions such as Take a pencil, put it under the book, and give me the scissors;
2) understanding of sentences, names, names of objects given in the form of descriptions.” Show what they use to cut bread, what they use to cut paper, what they use to light firewood, etc. (according to the corresponding pictures).
Difficulties in understanding multi-unit instructions are observed in all forms of aphasia with severe speech disorder.
6) examination of the understanding of grammatical structures,
proverbs, sayings, fables.
The patient is presented with the following tasks: Tell me, how do you understand the phrases “father’s brother” and “brother’s father”? Is this the same person or different people? If different, then who are they?
When showing the corresponding pictures, the speech therapist asks the patient to show
his mother’s daughter, daughter’s mother, daughter’s mother, mother’s daughter
.
In the same way, but relying on objects, the patient is asked to show a brush with a pencil, a pencil with a brush.
Testing the understanding of logical and grammatical constructions that convey the spatial arrangement of objects
, carried out by tasks: Place the pen to the right of the ruler and to the left of the pencil, the ruler to the left of the glasses correction key, etc.; Draw a cross under the circle, a circle above the cross, a cup under the table and above the Christmas tree, etc. To make the task easier, the patient is given schematic examples of these drawn objects.
When solving a task of a defining nature, the patient is asked to place the names of the children under the pictures: Kolya is higher than Vanya and lower than Sasha. Who are Kolya, Vanya and Sasha here? Or: Olya is darker than Katya and lighter than Tanya. Which of the girls is Olya, Katya and Tanya? Petya hit Kolya. Who's the fighter?
These tasks are difficult with afferent aphasia, and the instructions: “Show the spoon with a pencil, the pencil with a pen,” etc. are difficult with efferent aphasia.
Patients with semantic aphasia are characterized by difficulties in performing both logical and grammatical constructions.
7) examination of expressive speech
begins already during the preliminary conversation. The speech therapist writes down all his questions and tasks, as well as the patient’s speech and facial reactions, for example, in the form of a fraction: above the line is a question, the content of the drawing about which the patient must report something, below the line is the patient’s speech production.
Examination of the articulatory part of speech
The articulatory link can be disrupted in different types of afferent motor and efferent motor aphasia, with dysarthria
.
The patient is asked to repeat the sounds in isolation, in words, in a sentence. With gross afferent motor aphasia,
either abundant searches for the articulatory structure of sound, or literal paraphasias, or replacement of the pronunciation of individual sounds with speech emboli can be observed.
The patient either pronounces sounds correctly, then replaces them with others, or cannot find the desired articulatory position. With relatively restored situational speech (for example, with so-called conduction aphasia), patients may have difficulty pronouncing individual sounds, but more often - when pronouncing syllables and words. With grossly impaired phonemic hearing in patients with acoustic-gnostic aphasia,
errors may also be observed when repeating individual sounds.
Moreover, these difficulties are accompanied by comments from patients. Difficulties in repeating individual sounds
in
sensory
are secondary in nature and are a consequence of impaired auditory control.
One of the features of the repetition of individual sounds in
afferent motor and acoustic-gnostic sensory aphasia
is the tendency to deafen voiced phonemes,
in afferent motor aphasia there is a tendency
to voiceless phonemes,
in acoustic-gnostic sensory aphasia
there is a tendency to deafen the phoneme,
in afferent motor aphasia
there is due to apraxia of the vocal cords, a tendency to voicing in acoustic-gnostic aphasia is due to an increased compensatory pre-superstructure of acoustic control.
Examination of automated types of speech
The patient is invited, together with the speech therapist, to sing the melody of a familiar song (with and without words), repeat the singing independently, list the days of the week, months of the year, and reproduce the ordinal count. If this is not available to the patient, then the words are pronounced in conjunction with it.
Examination of conjugate and reflected repetition
allows us to clarify the degree of decay of phonemic hearing, auditory-verbal memory, articulatory praxis and the presence of perseveration in the speech of patients.
Patients are given the task to repeat several one-syllable, two-syllable, three-syllable and polysyllabic words of varying frequencies, as well as repeat phrases of varying lengths.
Examination of the nominative function of speech
Naming refers to reproductive, voluntary types of speech (repetition, dictation, reading aloud). Therefore, when starting the examination, the speech therapist asks the patient to name objects or images in one word, to find a categorical name (dishes, furniture).
Examination of dialogic and monologue speech
(preliminary conversation) The speech therapist notes whether the patient is verbose or not. How developed is his speech, does he speak in monosyllables, in separate lines, or uses cliche-like turns of phrase? Is there agrammatism in his situational speech, what is the nature of this agrammatism. To examine narrative speech, the patient is asked to compose sentences or a story based on plot pictures.
When recording the patient’s speech, the speech therapist notes the nature of the patient’s agrammatism, the richness of his vocabulary, verbal and literal paraphasias, preservation of the narrative plan, etc. With severe afferent and efferent aphasia, the patient’s narrative speech may be completely absent, and at an early stage with acoustic-gnostic aphasia be overloaded with literal paraphasias.
Examination
of the state of reading and writing
When examining the state of reading, special attention is paid to the possibility of internal reading
in speechless patients with afferent and efferent motor aphasia and sensory and acoustic-gnostic aphasia. Examination of the safety of internal reading to oneself in speechless patients is carried out using the following methods: 1) laying out captions for objects, plot pictures and series of pictures; 2) showing a word or sentence perceived by ear; 3) following written instructions: Show where the window is, Wag your finger, etc.
In patients complaining of reading difficulties with intact situational speech, it is necessary to check visual acuity and optical gnosis, the presence of hemianopsia (narrowing of the visual field, often observed in sensory aphasia). When studying reading capabilities in patients with moderate severity of speech disorders, the speech therapist notes literal and verbal paralexias, elements of guessing reading, perseveration, etc.
When examining writing and written speech, patients with severe speech disorder are asked to write individual sounds and short words under dictation (house, ear, window). In cases where the patient can cope with writing easy words, he is asked to write down words with consonant clusters (tail, friend, table) and polysyllabic words (for example: room, plane, chase). If the patient writes (with errors) individual words, he is asked to take dictation of simple and complex sentences, for example: Children go to the forest. The weather is bad outside, the journey ended well.
For mild speech disorder
There are errors in patients' letters. If the patient did not make mistakes when writing from dictation, it is necessary to move on to the study of written naming, composing a phrase or text based on plot pictures.
Impairments in written speech in all forms of aphasia are secondary to the primary disorder. In the written speech of patients with afferent motor aphasia, literal paraphasia is predominantly observed when recording sounds that are close in place and method of formation; in efferent aphasia - omission of vowels, rearrangements and perseveration of letters and syllables from previous words; in acoustic-gnostic aphasia - mixing of voiced and voiceless consonants etc. With rough and moderate severity of agraphia with afferent motor, efferent motor and acoustic-gnostic aphasia, omissions of consonants are observed at confluences of consonants in a syllable or at the junctions of syllables. In severe acoustic-gnostic aphasia at the very early stage of the disease, due to impaired auditory control, the patient can write extra letters in a word, repeat syllables, lengthening, for example, a word consisting of three letters to 8-12 letters. The speech therapist records the patient’s written speech also in the form of a fraction.
And finally, the speech therapist examines the patient’s integrity of counting operations
, offering to write down simple and multi-digit numbers, solve examples within 10, 100, 1000. Usually, seriously ill patients are given written examples like: 31 -17 (with a transition through ten), patients are asked to verbally subtract from 100 by seven, etc.
The examination of speech functions is carried out delicately
In order not to injure the patient, the patient is encouraged to overcome difficulties during the examination. The patient should leave the speech therapist encouraged, not overtired, and therefore the initial examination is carried out in a reduced manner and the speech status is clarified during repeated meetings.
Conclusion about the patient’s speech status
1) emotional and volitional traits of the patient, contact, integrity of personality, his orientation in place and time, attitude towards his speech defect, the presence of left-handedness in the patient and family members;
2) features of understanding situational speech, implementation of single- and polysyllabic instructions, auditory-speech memory, phonemic hearing, alienation of the meaning of a word, perseveration in completing tasks, understanding of logical-grammatical structures;
3) features of expressive speech: verbosity, aspontaneity, echolalia, perseveration, speech emboli, the nature of agrammatism, the presence of verbal and literal paraphasia, amnestic difficulties, oral or articulatory praxis. Possibilities of repetition, naming, composing phrases, automated speech. Is there a dissociation between reproductive voluntary and situational active speech, as well as the presence of dysarthria?
4) features of reading and writing: preservation of visual gnosis, letter recognition, features of reading silently and aloud, literal and verbal paraphasias, the ability to follow written instructions, global reading of individual words;
5) features of written speech disorders: writing individual letters, words under dictation, writing naming objects and their images, writing complex words and individual sentences under dictation, writing sentences based on a plot picture, the nature of literal and verbal paraphasia, agrammatism in written speech, character other defects in the patient's letter;
6) features of counting disorders: the ability to solve various arithmetic examples, write numbers under dictation;
7) features of gnosis and praxis: the presence of acoustic or optical agnosia, specularity in writing, oral and articulatory apraxia, dynamic and constructive-spatial apraxia, dysarthria, echolalia.
After a summary description of the patient’s speech status, a conclusion
, which notes
the form of aphasia, its degree of severity, the complexity of the two forms, the severity of agraphia, alexia, the nature of apraxia, the presence of left-handedness in the family, the degree of activity or aspontaneity , the presence of depression, efficiency, weak soul , disinhibited femininity).
Treatment methods
To eliminate aphasia, two directions are used - speech therapy and medical. The neurologist prescribes a course of medications that dilate blood vessels, improve metabolism and blood circulation. Additional means stimulate the functioning of the nervous system - these are physical therapy, massage, physiotherapy.
Aphasia can be characterized by different manifestations, so the speech therapist prepares correctional work based on the individual characteristics of the patient. The work is carried out under the supervision of the attending physician, since the deterioration of the child’s condition (decreased speech functions) indicates an increase in blood pressure and the development of other problems.
The first classes last 10 minutes, gradually increasing the time. It is important not to overload the patient. A personal notebook is created for each child, where information about the lesson is recorded.
Group classes are used whenever possible. They restore the communicative function of speech, remove phobias and fears. Children are selected in groups of 3-4 with approximately the same degree of defect. For sensory learners, groups consist of 2-3 people.
For motor aphasia, everyday themes and home dramatizations are widely used. At the beginning of the lesson, the speech therapist clearly outlines the lesson plan.
There are special kindergartens for preschool children, and a Type V school for schoolchildren. In educational institutions they are provided with all the necessary assistance.
Features of speech therapy assistance
It will take about five years of hard work to eliminate the disorder in adolescents. Only with a clear awareness of the defect and the desire to cope with it can significant improvement be achieved. Due to their age, children do not always understand the seriousness of the situation; they hope for a spontaneous cure and do not see the need for systematic treatment.
A specialist needs to develop all types of mental activity, develop motivation, the ability to plan, and practice movements. Every lesson should be interesting.
All material is selected taking into account the age of the child. For preschoolers and primary schoolchildren, modeling, design, drawing, and games are used. Children in the preparatory group are taught to read, write, form words from a split alphabet, and are given the basics of sound-letter analysis.
Schoolchildren have difficulties with orientation in time and space. Therefore, work is being done to develop mathematical concepts. Teenagers also have their foreign language skills restored.